|
Case Report
Microcystic/reticular schwannoma of the lower leg: Case report with review of literature
1 Department of Human Pathology, Juntendo University School of Medicine, Tokyo 113-8421, Japan
2 Intractable Disease Research Center, Juntendo University, Graduate School of Medicine, Tokyo 113-8421, Japan
3 Department of Medicine for Orthopaedics and Motor Organs, Juntendo University School of Medicine, Tokyo 113-8421, Japan
Address correspondence to:
Tsuyoshi Saito
MD, PhD, Department of Human Pathology, Juntendo University School of Medicine, Tokyo 113-8421,
Japan
Message to Corresponding Author
Article ID: 100063Z11TS2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Saito T, Kubota D, Sasa K, Hasegawa N, Hayashi T, Takagi T, Ishijima M. Microcystic/reticular schwannoma of the lower leg: Case report with review of literature. J Case Rep Images Pathol 2022;8(2):1–5.ABSTRACT
Introduction: Microcystic/reticular schwannoma is a distinctive histopathological variant of schwannoma, which is rare. Its occurrence in the subcutaneous soft tissue of the lower extremity has rarely been reported.
Case Report: We report a microcystic/reticular schwannoma arising from a subcutaneous lesion on the lower leg of a 33-year-old man. The patient noticed a subcutaneous mass on the right lower leg six months before admission and experienced radiation pain in the left lower leg. Magnetic resonance imaging revealed a well-demarcated mass with 11-mm maximum diameter with low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging in the subcutaneous region of the right lower leg. Histological examination revealed a cellular area at the periphery of the tumor, although the majority of the tumor showed a microcystic/reticular structure within the myxo-collagenous stroma. The current case was well capsulated and did not show an infiltrative growth pattern. In addition, aggregation of foamy macrophages was frequently seen, although it was reported as a rare feature. After complete surgical excision with clean resection margins, the patient is well, with no evidence of tumor recurrence on follow-up after postoperative 14 months.
Conclusion: In this case, infrequent findings for microcystic/reticular schwannoma were observed, although the presence of the classical Antoni A area was helpful for the diagnosis of microcystic/reticular schwannoma.
Keywords: Foamy cells, Lower extremity, Microcystic/reticular schwannoma, S-100
Introduction
Schwannoma is a slow-growing, solitary, and benign peripheral nerve sheath tumor derived from Schwann cells [1],[2]. It usually arises in the fourth or fifth decade of life in the subcutaneous tissue of the distal extremities, or in the head and neck region of adult patients, with no sex predilection [3],[4],[5]. Schwannomas also occur in a broad variety of anatomical regions, such as the mediastinum, gastrointestinal tract, retroperitoneum, spinal cord, cerebellopontine angle, and bone. Besides those arising in neurofibromatosis type 2, most schwannomas are solitary and sporadic lesions, although a small percentage of cases may be associated with von Recklinghausen’s disease [6]. Conventional schwannomas are usually encapsulated lesions that are histologically characterized by a biphasic growth pattern, traditionally designated by Antoni A areas (highly ordered cellular component showing typical nuclear palisading) and Antoni B areas (hypocellular myxoid component). A common feature of both components is the presence of thick-walled hyalinized vessels. The tumor cells showed strong cytoplasmic and nuclear staining for S-100 protein. In addition to the classic type, at least 11 different histopathological subtypes have been described [6]. These variants include ancient (degenerated) schwannoma [7], cellular schwannoma [8], and these two variants are the most major ones. In addition, plexiform schwannoma [9], melanotic schwannoma [10],[11], epithelioid schwannoma [12], hybrid schwannoma/neurofibroma [13], hybrid schwannoma/perineurioma [14], gastrointestinal schwannoma [15], neuroblastoma-like schwannoma [16], lipoblastic schwannoma [17], and microcystic/reticular schwannoma are also reported [18]. All of these histopathological variants highlight the morphological heterogeneity of schwannomas. Microcystic/reticular schwannomas tend to occur in the gastrointestinal tract [19]. Unawareness of these uncommon histopathological variants may lead to diagnostic pitfalls and the risk of mistreatment due to misdiagnosis. In particular, for microcystic/reticular schwannomas, malignant neoplasms such as signet ring cell carcinoma and mucous carcinoma often need to be carefully ruled out. Furthermore, rare cases of microcystic/reticular schwannoma in the subcutaneous soft tissue and thoracic cavity have been reported [20],[21]. However, the occurrence on the lower extremity seems to be quite rare. We report a case of a microcystic/reticular schwannoma arising from a subcutaneous lesion on the lower leg.
Case Report
Clinical history
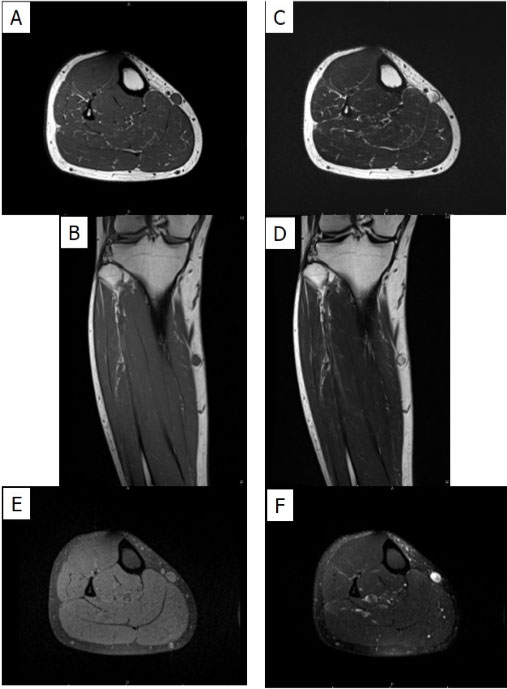
A 33-year-old Japanese man was referred for a subcutaneous mass in the right lower leg that had lasted for eight months. The tumor gradually increased in size. He had no significant past medical history, including a malignant neoplasm. There was association with Neurofibromatosis 1 or 2. Radiating pain was observed from the mass. Plain radiography did not reveal any lesion. However, magnetic resonance imaging revealed a well-demarcated mass with 11-mm maximum diameter with low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging in the subcutaneous region of the right lower leg (Figure 1A, Figure 1B, Figure 1C, Figure 1D, Figure 1E, Figure 1F). Based on these findings, a benign neurogenic tumor was suspected. The tumor was resected and sent for a pathologic diagnosis.
Pathology
The resected subcutaneous tumor measured 12 mm × 12 mm × 5 mm. Histologically, the tumor was encapsulated by thin fibrous tissue (Figure 2A). Lobulation was not observed. Cellular area was observed only at the periphery of the tumor, where the spindle-shaped cells proliferated in a fascicular fashion and frequently showed nuclear palisading (Figure 2B). A microcystic/reticular pattern with myxoid stroma was observed at the center of the tumor (Figure 2C and Figure 2D). Aggregates of foamy macrophages, often accompanied by lymphocytic infiltration, are also frequently observed (Figure 2E). Cystic changes were prominent at the center of the tumor (Figure 2F). Nuclear pleomorphism was not evident and necrosis was not observed. Hyalinized blood vessels were not observed; mitotic figures were also not observed. Immunohistochemistry (IHC) was performed using DAKO Autostainer Link 48 (Agilent, Santa Clara, CA) or manually stained with antibodies against the S-100 protein (Clone EP32; 1:800; Leica Biosystems), EMA (Clone E29, DAKO), CD1a (Clone EP32, DAKO), CD68 (Clone PG-M1, DAKO), MUC4 (8G7, sc-53945, Santacruz Biotechnology). The tumor cells were diffusely and strongly positive for S-100 protein (Figure 2G), but negative for EMA and MUC4. Based on these findings, the patient was diagnosed with a microcystic/reticular schwannoma.
Follow-up
After complete surgical excision with clean resection margins, the patient is well, with no evidence of tumor recurrence on follow-up after postoperative 14 months.
Discussion
We encountered a rare case of microcystic/reticular schwannoma on the lower leg in a young adult male. The microcystic/reticular schwannoma variant was initially described in 2008 by Liegl et al. as a distinctive histopathological variant of schwannoma, with predilection for visceral locations, particularly for the gastrointestinal tract [18], although schwannoma with only focal reticular growth pattern has been described previously as ‘‘focally rare features’’ in otherwise typical schwannomas [22]. This variant of schwannoma is reported to be the rarest subtype of schwannoma and preferentially occurs in the visceral site, most commonly in the gastrointestinal tract [1] and in their study only 3 of 10 cases occurred in soft tissues, two of which were located in the subcutaneous tissue [18]. A recent nice review demonstrated that there have been eight microcystic/reticular schwannomas of subcutaneous/soft tissue origin reported [23]. Six of those eight tumors were at least partially encapsulated as this case [23]. Microcystic/reticular schwannoma reportedly tends to represent a solitary, non-painful papule or nodule measuring 0.5–2 cm in the largest diameter (mean: 0.9 cm, median: 0.7 cm) [18],[24],[25], which is consistent with this case. Furthermore, this tumor tends to occur at a relatively older age [18] or in adults in the fifth decade of life (mean: 42.1 years, median, 42 years) [24],[25], although the recent review reports four cases younger than 30-year old [23]. In addition, this rarest type of schwannoma tends to show predilection for the upper extremities and back [18],[24],[25]. The recent review paper also demonstrated that all extremity cases occurred at upper extremity but not at lower extremity [23]. At least in terms of location, this case seemed to occur at a rather rare location (lower leg). This variant of schwannoma often shows an Antoni A cellular area within the tumor [22]. Our case also contained a cellular area at the periphery of the tumor, although the majority of the tumors showed a microcystic/reticular structure within the myxo-collagenous stroma. The presence of the classical Antoni B area at the periphery of microcystic/reticular schwannomas has also been reported [25]. The presence of the classical Antoni A area in the current case was helpful in the diagnosis of microcystic/reticular schwannoma without extensive ancillary studies. Unlike classic schwannoma, the reticular variant may lack encapsulation [18],[25] and reveal a bizarre microcystic and/or reticular architecture, containing focal infiltrative areas [18]. The current case was well capsulated and did not show an infiltrative growth pattern. In addition, aggregation of foamy macrophages was generally absent; however, this was frequently observed in this case.
Regarding the differential diagnosis, several tumors could be raised. Hybrid reticular perineurioma/schwannoma occurs sporadically, while hybrid neurofibroma/schwannoma is strongly associated with neurofibromatosis. Perineurial cells with slender nuclei were not observed and storiform pattern was not identified throughout the lesion. Furthermore, EMA IHC did not show positive cells, thus hybrid reticular perineurioma/schwannoma was ruled out. Low-grade fibromyxoid sarcoma (LGFMS) also needs to be carefully differentiated especially from biopsy specimen. The reticular/microcystic pattern within myxoid stroma might be reminiscent of the short fascicular pattern of spindle cells observed in LGFMS. Fibrous stroma was not evident in this tumor and MUC4 IHC was totally negative, denying the possibility of LGFMS. Soft tissue metastasis of signet ring cell carcinoma might be also considered in case of previous history of signet ring cell carcinoma. This patient did not have such medical history.
Conclusion
We encountered a case of subcutaneous microcystic/reticular schwannoma of the lower extremity at a rare location as a tumor. Awareness of this rare variant of schwannoma could avoid a misdiagnosis and overtreatment.
REFERENCES
2.
Kurtkaya-Yapicier O, Scheithauer B, Woodruff JM. The pathobiologic spectrum of schwannomas. Histol Histopathol 2003;18(3):925–34. [CrossRef]
[Pubmed]

3.
Das Gupta TK, Brasfield RD, Strong EW, Hajdu SI. Benign solitary schwannomas (neurilemmomas). Cancer 1969;24(2):355–66. [CrossRef]
[Pubmed]

4.
Dahl I, Hagmar B, Idvall I. Benign solitary neurilemmoma (schwannoma). A correlative cytological and histological study of 28 cases. Acta Pathol Microbiol Immunol Scand A 1984;92(2):91–101.
[Pubmed]

5.
Hennessee MT, Walter JH Jr, Wallace G, Lemont H, Quintavalle PR Jr. Benign schwannoma. Clinical and histopathologic findings. J Am Podiatr Med Assoc 1985;75(6):310–4. [CrossRef]
[Pubmed]

6.
Tang SX, Sun YH, Zhou XR, Wang J. Bowel mesentery (meso-appendix) microcystic/reticular schwannoma: Case report and literature review. World J Gastroenterol 2014;20(5):1371–6. [CrossRef]
[Pubmed]

7.
Dahl I. Ancient neurilemmoma (schwannoma). Acta Pathol Microbiol Scand A 1977;85(6):812–8. [CrossRef]
[Pubmed]

8.
Casadei GP, Scheithauer BW, Hirose T, Manfrini M, Van Houton C, Wood MB. Cellular schwannoma. A clinicopathologic, DNA flow cytometric, and proliferation marker study of 70 patients. Cancer 1995;75(5):1109–19. [CrossRef]
[Pubmed]

9.
Kao GF, Laskin WB, Olsen TG. Solitary cutaneous plexiform neurilemmoma (schwannoma): A clinicopathologic, immunohistochemical, and ultrastructural study of 11 cases. Mod Pathol 1989;2(1):20–6.
[Pubmed]

10.
Carney JA. Psammomatous melanotic schwannoma. A distinctive, heritable tumor with special associations, including cardiac myxoma and the Cushing syndrome. Am J Surg Pathol 1990;14(3):206–22.
[Pubmed]

11.
Font RL, Truong LD. Melanotic schwannoma of soft tissues. Electron-microscopic observations and review of literature. Am J Surg Pathol 1984;8(2):129–38. [CrossRef]
[Pubmed]

12.
Kindblom LG, Meis-Kindblom JM, Havel G, Busch C. Benign epithelioid schwannoma. Am J Surg Pathol 1998;22(6):762–70. [CrossRef]
[Pubmed]

13.
Feany MB, Anthony DC, Fletcher CD. Nerve sheath tumours with hybrid features of neurofibroma and schwannoma: A conceptual challenge. Histopathology 1998;32(5):405–10. [CrossRef]
[Pubmed]

14.
Yang X, Zeng Y, Wang J. Hybrid schwannoma/perineurioma: Report of 10 Chinese cases supporting a distinctive entity. Int J Surg Pathol 2013;21(1):22–8. [CrossRef]
[Pubmed]

15.
Hou YY, Tan YS, Xu JF. Schwannoma of the gastrointestinal tract: A clinicopathological, immunohistochemical and ultrastructural study of 33 cases. Histopathology 2006;48(5):536–45. [CrossRef]
[Pubmed]

16.
Fisher C, Chappell ME, Weiss SW. Neuroblastoma-like epithelioid schwannoma. Histopathology 1995;26(2):193–4. [CrossRef]
[Pubmed]

17.
Plaza JA, Wakely PE Jr, Suster S. Lipoblastic nerve sheath tumors: Report of a distinctive variant of neural soft tissue neoplasm with adipocytic differentiation. Am J Surg Pathol 2006;30(3):337–44. [CrossRef]
[Pubmed]

18.
Liegl B, Bennett MW, Fletcher CDM. Microcystic/reticular schwannoma: A distinct variant with predilection for visceral locations. Am J Surg Pathol 2008;32(7):1080–7. [CrossRef]
[Pubmed]

19.
Chetty R. Reticular and microcystic schwannoma: A distinctive tumor of the gastrointestinal tract. Ann Diagn Pathol 2011;15(3):198–201. [CrossRef]
[Pubmed]

20.
Georgescu TA, Dumitru AV, Oproiu AM, et al. Cutaneous microcystic/reticular schwannoma: Case report and literature review of an exceedingly rare entity with an unusual presentation. Rom J Morphol Embryol 2018;59(1):303–9.
[Pubmed]

21.
Lau PP, Yau DTW, Lau WH, Mak LS, Chan JKC. Multinodular reticular schwannoma in the head and neck region: A potential diagnostic pitfall. Int J Surg Pathol 2013;21(1):54–8. [CrossRef]
[Pubmed]

22.
23.
Liu C, Yan L, Liu Q, et al. Lumbar intraspinal microcystic/reticular schwannoma: Case report and literature review. Medicine (Baltimore) 2018;97(39):e12474.
[Pubmed]

24.
Lisle A, Jokinen C, Argenyi Z. Cutaneous pseudoglandular schwannoma: A case report of an unusual histopathologic variant. Am J Dermatopathol 2011,33:e63. [CrossRef]
[Pubmed]

25.
Luzar B, Tanaka M, Schneider J, Calonje E. Cutaneous microcystic/reticular schwannoma: A poorly recognized entity. J Cutan Pathol 2016;43(5):93–100. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Tsuyoshi Saito - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Daisuke Kubota - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Keita Sasa - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Nobuhiko Hasegawa - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Takuo Hayashi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Tatsuya Takagi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Muneaki Ishijima - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Tsuyoshi Saito et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.