|
Case Report
Primary liver yolk sac tumor with lung metastasis in adolescence: Rare case report
1 Faculty of Medicine, University of Ottawa, Ottawa, Ontario, Canada
2 Department of Health Sciences, Carleton University, Ottawa, Ontario, Canada
3 Department of Laboratory Medicine, Children’s Hospital of Eastern Ontario, Ottawa, Ontario, Canada
4 Faculty of Medicine, Libyan International Medical University, Benghazi, Libya
5 Department of Pathology, The Ottawa Hospital, Ottawa, Ontario, Canada
Address correspondence to:
Joseph de Nanassy
Pediatric Pathologist, Children’s Hospital of Eastern Ontario, 401 Smyth Rd, Ottawa, ON K1H 8L1,
Canada
Message to Corresponding Author
Article ID: 100081Z11YN2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Nasr Y, Mehdi S, Tristani L, Alowami M, Chernetsova E, de Nanassy J. Primary liver yolk sac tumor with lung metastasis in adolescence: Rare case report. J Case Rep Images Pathol 2024;10(2):22–26.ABSTRACT
Introduction: Germ cell tumors (GCTs) often arise within the gonads but occasionally appear within the extragonadal areas. Yolk sac tumors (YSTs), a type of GCT, are most often found in infants and adolescents due to puberty. However, primary liver YST cases are rare, with only one other reported case in the adolescent population.
Case Report: The current case examines a 15-year-old female patient experiencing significant weight loss, respiratory issues, and fevers. After her blood work displayed high alpha-fetoprotein (AFP) levels, a biopsy revealed a stage four primary liver YST with lung metastasis. The infrequency and primary location of the tumor, combined with her age, create challenges in diagnosis and treatment. Due to its rarity, the reporting of this case may aid in diagnosis when encountered. We highlight and present our experience of management and prognosis of primary-hepatic YST when encountered in adolescents.
Conclusion: At two years follow-up, the patient showed no evidence of recurrence or metastasis.
Keywords: Germ cell tumor, Hepatic metastasis, Immunohistochemistry, Pediatric, Yolk sac tumor
Introduction
Germ cell tumors (GCTs) are neoplasms involving germline cells [1]. They commonly arise within the gonads (testes and sometimes the ovaries) but can occasionally appear as extragonadal GCT—often occurring within the central nervous system (e.g., brain and sacral region, or mediastinum and retroperitoneum regions) [2],[3],[4]. However, in even more unique instances, GCTs arise within other organs such as the liver [2],[3]. While GCTs are rare, they tend to more commonly occur in young children, as compared to adults, comprising roughly 3% of all childhood neoplasms (ages 0–18 years) [3],[5],[6],[7]. Current literature suggests that there are two time periods of increased incidence in GCT development: during infancy (0–4 years of age) and the beginning of puberty (12–18 years of age) [1]. Such findings explain the rise in GCT incidence concerning puberty as they account for 11–15% of adolescent cancers [1],[3],[5].
Germ cell tumors are divided into two histological categories: seminomatous and nonseminomatous GCTs [1]. Nonseminomatous GCTs are further divided into separate categories, one of which includes yolk sac tumors (YST) [1]. Most treatments for pediatric GCTs are based on clinical trials examining testicular GCTs in adults, often not including pediatric GCTs [1]. Therefore, current knowledge is based on adults testicular GCT management protocols, potentially not addressing the conceivable biological differences and clinical behavior of pediatric GCTs.
Past literature has reported GCT of the primary liver, but tumors to the hepatic parenchyma more often arise through metastases from gonadal GCTs [8],[9]. For instance, in 2003, fewer than 20 cases were reported, most of which involved infants and young children [7],[9]. Therefore, their unlikely nature and uncommonness within adolescents make primary liver GCTs challenging to diagnose and treat due to limited current knowledge.
The current case involves a 15-year-old girl presenting with a rare extragonadal GCT primary to the liver with lung metastasis and YST components. This case report and review shed light on a very unusual cases of primary YST in the liver occurring in adolescent, highlighting the salient presentation, histological and genetic findings, and outcomes.
Case Report
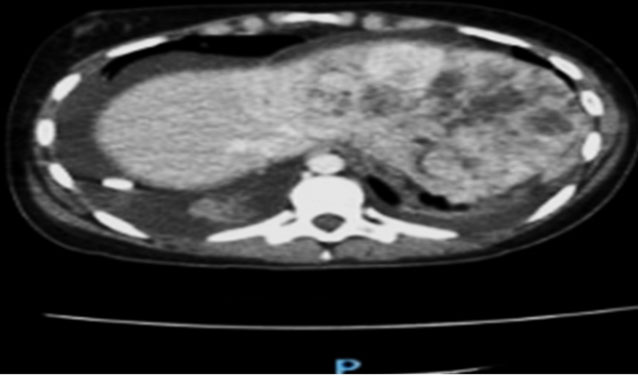
We report a 15-year-old female patient presented with respiratory issues, and fevers due to COVID-19. She had a protracted convalescing period; however, never fully returned to complete health. Afterward, she developed a productive cough, shortness of breath, chest pain, constipation, dizzy spells, intermittent fevers (at 102°F), night sweats, headaches, arthralgias, back pain and myalgias, constant nausea, loss of appetite, and weight loss. Initial blood work revealed, leukocytosis (15.4 normal value: 3.5–10.5 × 109/L), neutrophilia (10.5 normal value 1.5–7.5 × 109/L), and thrombocytosis (520 normal value 130–380 × 109/L). The patient was seen by the emergency physician, and was found to have mediastinal, hilar lymphadenopathy, and right pleural effusion. Laboratory investigations at that time showed elevated fibrinogen levels (7.27 normal value .70–3.50 g/L), low albumin (28 normal value 38–50 g/L), elevated alanine aminotransferase (ALT) (130 normal ≤24 U/L), aspartate aminotransferase (159 normal <31 U/L), gamma-glutamyl transferase (GGT) (40 normal ≤17 U/L), and anaplastic lymphoma kinase (ALK) (113 normal 54–93 U/L) a significant increase in serum alpha-fetoprotein (AFP) (191 with expected reference of 40). The abdominal and pelvic computed tomography (CT) revealed a large soft tissue and necrotic intra-abdominal mass, occupying most of the left lobe of the liver (Figure 1). Differential included hepatocellular carcinoma (HCC), angiosarcoma, or synovial sarcoma of the peritoneum. Numerous lung nodules and masses, along with moderate right pleural effusion, mediastinal and hilar lymphadenopathy, were suggestive of metastasis (Figure 2). Indeterminant cyst at the region of the pancreatic head was also noted. Imaging differentials included hepatocellular carcinoma, angiosarcoma, or synovial sarcoma of the peritoneum. Infection was a less likely consideration as the scattered multiple soft tissue nodules along the peritoneal surfaces are suggestive of peritoneal metastases.
A core needle biopsy of the left hepatic lobe and lung revealed similar microscopic findings of a partially necrotic tumor (Figure 3 and Figure 4). They showed polygonal epithelioid cells with marked nuclear pleomorphism, prominent nucleoli, and clear to eosinophilic cytoplasm. There was evidence of focal glandular differentiation. Immunochemistry showed the neoplastic cells were positive for AE1/3, Ber-EP4, CK8/18, Glypican 3, Keratin 903, INI-1 (retained), and SALL4. Beta-catenin showed cytoplasmic staining only. The tumor cells were also focally positive for CDX2, CK7, and inhibin. The tumor cells were negative for CK20, EMA, arginase, calretinin, monoclonal CEA, CD10, CD30, CD31, CD34, CD56, CD117, chromogranin, glutamine synthetase, MelanA, Oct ¾, PLAP, S100, synaptophysin, TTF-1, and WT-1. The patient was diagnosed with a stage 4 GCT of primary left liver lobe and lung metastasis.
The diagnosis allowed for the patient to be enrolled within Precision Oncology for Young People (PROFYLE), a Canadian precision medicine research institute. Precision Oncology for Young People profiles rare cancers in children and young adults through genomic sequencing including patients’ tumors and blood [10],[11].
Initial treatment involved hormonal therapy (i.e., suppressing the patient’s menstrual cycle with letrozole and leuprolide) as a means of slowing tumor growth [12]. The patient underwent multiple rounds of bleomycin, etoposide, cisplatin (BEP) chemotherapy, and high carboplatin and etopophos (EP) chemotherapy. The patient also received two separate autologous stem cell rescue transplants.
Follow-up CT with contract revealed interval decrease in the size of the left liver mass. Decreased size of the cystic lesion was seen at the pancreatic head/body junction; significantly improved peritoneal metastases. Interval decreased in size of the innumerable bilateral pulmonary metastatic nodules. A single new pulmonary nodule was seen in the upper segment of the left lower lobe. Almost completely resolved right pleural effusion.
A seven-month follow-up biopsy revealed an entirely necrotic tumor with only an isolated microscopic focus of a few residual viable liver tumor. These rare residual viable cells were atypical cells and stained positive for SALL4, consistent with a minute focus of few residual tumor cells indicating an excellent response to treatment. Imaging studies revealed no presence of residual lung metastasis. The patient remains alive and continues with chemotherapy and follow-up CT scans. During the two years of follow-up, the patient showed no evidence of recurrence or metastasis.
Discussion
Extragonadal GCTs, specifically those within the liver, are extremely rare [7],[9]. Of the limited available cases on the literature, we only identified one additional case of primary YST arising in the liver of an adolescent (Table 1). The rare nature and limited knowledge regarding primary liver YST poses incredible challenges for diagnosis and effective treatment of these tumors.
Our case of the primary liver YST and the only additional identified case in the literature occurring in adolescents [6] show similarities between patient sex, age, tumor presentation and immunochemical staining (Table 2). For instance, both cases involve a female patient. This aligns with previous literature that suggests extragonadal adolescent YSTs are more common within female patients as there is a hormonal influence on the tumor [4],[6],[13]. Furthermore, in both cases, the patient was diagnosed within pubertal years (15 years of age and 13 years of age, respectively).
Unlike the case reported by Fanelli et al. [6], the presence of metastasis in the current case did not allow for complete surgical resection. However, basal ganglia disease, which impacts the brain’s ability to navigate changes in movement, complicated the 2019 case, a side effect not found in the current case [6]. After resection, the patient began chemotherapy which resulted in decreased AFP levels [6]. But soon afterward, they rose again, requiring the return of regular chemotherapy [6]. Three months after resection, the 2019 patient died from febrile neutropenia and pulmonary infection, a complication to her chemotherapy [6].
Conclusion
Primary liver YSTs are rare tumors and are extremely rare in adolescents. We present a 15-year-old female patient with primary liver YST. At two years follow-up, the patient shows no recurrence or metastasis. Our literature review identified only one additional case to our own of primary liver YST in the adolescent population, who died three months from presentation and start of treatment. Awareness of the features of primary liver YSTs in adolescents will aid in diagnosis and treatment of future cases.
REFERENCES
1.
Pierce JL, Frazier AL, Amatruda JF. Pediatric germ cell tumors: A developmental perspective. Adv Urol 2018;2018:9059382. [CrossRef]
[Pubmed]

2.
Rosti G, Secondino S, Necchi A, Fornarini G, Pedrazzoli P. Primary mediastinal germ cell tumors. Semin Oncol 2019;46(2):107–11. [CrossRef]
[Pubmed]

3.
Poynter JN, Fonstad R, Tolar J, Spector LG, Ross JA. Incidence of intracranial germ cell tumors by race in the United States, 1992–2010. J Neurooncol 2014;120(2):381–8. [CrossRef]
[Pubmed]

4.
Vanidassane I, Sharma V, Ramteke P, Yadav MK, Batra A. Primary yolk sac tumor of the liver in an adult man. ACG Case Rep J 2019;6(4):e00050. [CrossRef]
[Pubmed]

5.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69(1):7–34. [CrossRef]
[Pubmed]

6.
Fanelli MCA, Duarte AAB, de Souza FKM et al. Primary germ cell tumor of the liver. Journal of Pediatric Surgery Case Reports 201951:101324 [CrossRef]

7.
Veneris JT, Mahajan P, Frazier AL. Contemporary management of ovarian germ cell tumors and remaining controversies. Gynecol Oncol 2020;158(2):467–75. [CrossRef]
[Pubmed]

8.
Litten JB, Tomlinson GE. Liver tumors in children. Oncologist 2008;13(7):812–20. [CrossRef]
[Pubmed]

9.
Verma M, Agarwal S, Mohta A. Primary mixed germ cell tumour of the liver – A case report. Indian J Pathol Microbiol 2003;46(4):658–9.
[Pubmed]

10.
Narod SA, Stiller C, Lenoir GM. An estimate of the heritable fraction of childhood cancer. Br J Cancer 1991;63(6):993–9. [CrossRef]
[Pubmed]

11.
Grover SA, Berman JN, Chan JA, et al. Abstract 5413: Terry fox precision oncology for young people (PROFYLE): A Canadian precision medicine program for children, adolescents and young adults with hard-to treat cancer. Cancer Res 2020;80(16_Suppl):5413. [CrossRef]

12.
Mitra S, Lami MS, Ghosh A, et al. Hormonal therapy for gynecological cancers: How far has science progressed toward clinical applications? Cancers (Basel) 2022;14(3):759. [CrossRef]
[Pubmed]

13.
Warren M, Thompson KS. Two cases of primary yolk sac tumor of the liver in childhood: Case reports and literature review. Pediatr Dev Pathol 2009;12(5):410–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Youssef Nasr - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Samira Mehdi - Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Lauren Tristani - Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Moaz Alowami - Analysis of data, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Elizaveta Chernetsova - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Joseph de Nanassy - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Youssef Nasr et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.